(none at this time)
In 2026, the Schizophrenia & Psychosis Action Alliance is launching the Solutions Series—a new national, multi-city event series focused on moving beyond conversation to action. Each gathering will bring together people with lived experience, families, clinicians, researchers, advocates, policymakers, and community partners to co-design practical, real-world solutions to the most urgent challenges in schizophrenia and psychosis care.
Join us on May 14 and 15 in Washington, D.C., for our 2nd annual SPRING Summit, where we’ll work together to plan and activate core components of our Roadmap to Recovery.
We’ll focus on the emotional and social isolation that causes traumatic stress, additional medical issues and lost productivity for people with schizophrenia and their care partners. This trauma affects everyone in the schizophrenia ecosystem – from diagnosed people’s ability to advocate for themselves, to the caregiver burden, to clinicians who may experience “compassion fatigue” that hinders treatment.
Learn about the implications of FDA’s momentous decision to eliminate its clozapine REMS restrictions.
We discuss what pharmacies, insurance companies, prescribers and others can do to help make clozapine accessible to the people who need it, and what people with schizophrenia can do in the meantime.
The announcement of the REMS removal has led to a flurry of questions among clozapine stakeholders about how to cut through the complicated web of insurance rules and other barriers that people with schizophrenia, prescribers and pharmacies have faced for years.

Bethany James
Living with schizophrenia
Matt Petersen
Caregiver

Dr. Kim Mueser
Clinician

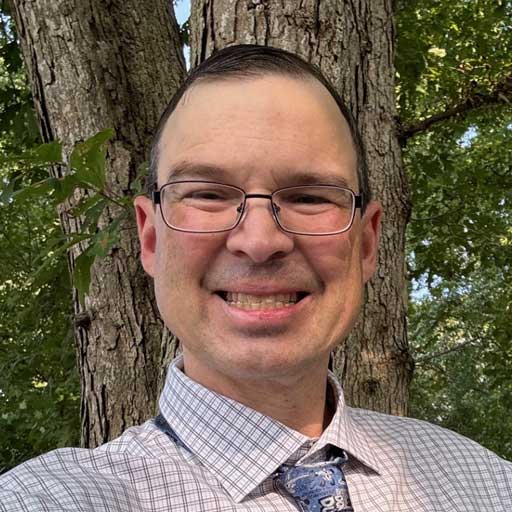
Dr. Peter Weiden, M.D.
Psychiatrist
The cognitive symptoms of schizophrenia can have a significant negative impact on a person’s employment, ability to attend school and social functioning. Cognitive problems can lead to social isolation, which can worsen symptoms and make relapses more likely. They also can prevent a person with schizophrenia from being able to live independently.
While cognitive impairment can be present even before the first symptoms appear, it is not always obvious. As a result, it’s not always considered a key component of schizophrenia or an important treatment target. In this webinar, a person diagnosed with schizophrenia, a caregiver and a clinician will discuss the real-world impact of cognitive symptoms and the importance of treating them to optimize a person’s ability to re-integrate into their social environment, school, work and society.
The negative symptoms of schizophrenia are common, debilitating and can be the biggest barrier to re-integrating into life after diagnosis. Yet most schizophrenia treatments have not addressed these serious symptoms, which include a lack of motivation, reduced emotional expression and a decreased ability to speak (or less interest in speaking).
In this recorded webinar, a person diagnosed with schizophrenia, a caregiver and a clinician discuss constructive ways to approach and manage negative symptoms. They also share clinician strategies for working with patients and their caregivers to understand the degree of burden negative symptoms are causing and design a treatment plan to address them.
Delusions, hallucinations and disorganized thinking are symptoms that contribute to the stigma and discrimination that those diagnosed with schizophrenia face every day. Yet these symptoms are described as “positive,” which on its face makes no sense.
The term actually has a mathematical source: positive symptoms are ADDED to what the general public experiences. Whatever their name, they can significantly affect a person’s ability to manage day-to-day life and are a main target of schizophrenia treatment.
Watch the recording of this webinar for a 360-degree perspective on the roles people living with the disease, caregivers and clinicians can play in managing these symptoms on the pathway to recovery.
S&PAA’s inaugural Schizophrenia Policy and Research Institute NextGen (SPRING) Summit in Washington, D.C., was a unique and groundbreaking collaboration of 125 people who represented the diverse range of stakeholders in the schizophrenia journey: those diagnosed with the disease, care partners, judges, law enforcement, researchers, community leaders and policymakers. Summit participants pinpointed the biggest barriers to schizophrenia treatment and recovery, then worked to identify solutions, launching a Roadmap to Recovery that will guide our collaborative efforts moving forward. True to the S&PAA mission, the voices of those impacted by the disease drove the discussions and helped guide the outcomes.
On World Schizophrenia Awareness Day, we launched a Day of Action to draw urgent public attention to the discrimination against people living with schizophrenia that is so embedded in our health systems and society. We hosted three major events to shine a light on these realities and help end this inequity:
Hill Day
Fly-In
We connected 30 people from our community with 31 members of Congress to advocate that funding be increased for programs to help people with schizophrenia survive and thrive.
Capitol Hill
Briefing
Capitol Hill staff joined families from our community at a briefing as we called for improving access to treatment.
Policy
Webinar
Nearly 300 people attended our Alliance for Health Policy webinar, during which experts discussed the severe gaps in care (e.g., medication management) and how to solve them.
People living with schizophrenia and other psychosis spectrum disorders are too often misunderstood or ignored, and current treatments are outdated and can cause significant side effects. On November 2, 2022, the schizophrenia community finally had the spotlight, as those living with the condition and their family members shared their treatment needs and concerns with drug developers and FDA staff.
The Externally-Led Patient Focused Drug Development (PFDD) meeting – “Reimagine Schizophrenia: Transforming How We Are Treated, Function and Thrive” – offered the chance to make what matters to those living with the neurobiological brain disease a higher priority in drug development and the FDA review process.
The meeting was co-hosted by the Schizophrenia & Psychosis Action Alliance, the American Foundation for Suicide Prevention, Mental Health America, the National Alliance on Mental Illness, and the National Council for Mental Wellbeing.
in-person
We will co-host this in-person lunch briefing on Capitol Hill with the American Association of Psychiatric Pharmacists. This event is for members of Congress and their staff, and will focus on the dangerous treatment barriers for people with schizophrenia.
The U.S. Food and Drug Administration issued a Risk Evaluation and Mitigation Strategies (REMS) program for clozapine in 2019. This program created severe restrictions on pharmacies and healthcare providers and resulted in grave danger to people with schizophrenia who rely on clozapine to manage their brain disease. It has led to patients losing access to the medication and suffering from severe psychosis – leading to hospitalization and worsened illness, loss of jobs and housing and in at least one case, death.
We are aligned with other leading stakeholder organizations, as well as with people living with schizophrenia and their families, to raise awareness of the consequences of the REMS and advocate for its modification or removal.
in-person
This is an exclusive opportunity to visit the U.S. Capitol and meet with Congressional members and legislative staff. It is an important chance for our community to engage directly with policymakers to share your experiences and drive conversations that will improve the lives of people with schizophrenia.
Our sign-up list is full! Thank you for your support.
virtual

This virtual webinar, hosted by the Alliance for Health Policy in partnership with S&PAA, will showcase the severe, systemic gaps in care, the resulting cost to individuals, families and society and the actions required to bridge those gaps. The event is targeted to government leaders, healthcare experts and housing and criminal justice audiences, but is open to all who are interested.
Click here to register.